Latest data from the Department of Health (DOH) stated that at least 2.6 million Filipinos have been fully vaccinated against COVID-19. According to herdimmunity.ph, this is only 3.76% of the 70-million population the government aims to vaccinate this year to achieve herd immunity. The website says that at the current average rate of 216,451 daily vaccinations, herd immunity will be reached in 1.6 years, or in February 2023. For us to achieve herd immunity by the end of the year, the government needs to ramp up its vaccination 3.3 times its current rate.
Herd immunity or population immunity is defined by the World Health Organization (WHO) as the “indirect protection from an infectious disease that happens when a population is immune either through vaccination or immunity developed through previous infection.” To better understand how we can reach this goal faster, the pilot online episode of Panayam sa Panahon TV featured the experts—health reform advocate Dr. Anthony Leachon and Dr. Noel Bernardo from the Philippine Red Cross.
 (photo from Quezon City Hall’s Facebook page)
(photo from Quezon City Hall’s Facebook page)
Why PH is falling behind in the global vaccination drive
When the COVID-19 vaccines still weren’t available, governments resorted to lockdowns to stop the spread of disease. But now, countries like the United Kingdom and the United States have freed up their economies, thanks to systematic and rapid vaccination programs. In a recent segment of Panahon TV called Buhay Pandemya, which featured a Filipino caregiver in Jerusalem in Israel, maskless locals can be seen flocking to the streets and celebrating the return of normalcy. Israel was one of the countries that started their vaccination early, which began last December 2020.
But the scenario in the Philippines is a different story. Though cases in the National Capitol Region (NCR) have been somewhat contained, other areas are experiencing surges. Lockdowns and quarantines are still in place, keeping the economy from fully recovering. If we already know the tried-and-tested formula of mass vaccination as the main key to herd immunity, why then are we still behind in the immunization drive? Our experts chalked it up to three main reasons.
- Lack of vaccine supply
Based on Our World in Data’s latest report, the Philippines ranks 8th among the 10 ASEAN countries in terms of vaccine rollout. During the interview, Dr. Bernardo expressed surprise over his discovery that out of the 3,700 approved vaccination sites in the country, only 1,700 are active. “Based on my experience on the ground with the different LGUs and the bakuna centers of the Philippine Red Cross, a big factor is the lack of vaccines,” he said in Filipino. “Bakuna centers don’t receive enough vaccines. Other LGUs (local government units) can only operate half-days.” Dr. Leachon was quick to agree. “If you don’t have vaccines, it doesn’t matter if you have vaccination sites. People will still have no access to vaccination.”
- Lack of organization
With data gathered from DOH, the National Task Force Against COVID-19, the Inter-Agency Task Force and news outlets, Herdimmunity.ph states that we currently have over 17 million vaccine doses, “enough to fully vaccinate 12.47% of the target population.” If such is the case, why is the vaccination still slow?
Dr. Leachon pointed out that LGUs have varying levels of governance, with some more organized than the others. Because best practices are not adopted by all LGUs, they also have varying levels of success, making it harder for the country to reach herd immunity.
Meanwhile, Dr. Bernardo said that we should attack the issue with a “system approach”. He cited how a simple step such as securing a vaccination schedule has become problematic. “People shouldn’t have to walk in like chance passengers. When we schedule them, we know that number one, they fully consent to the vaccination. Second, they should know their vaccine brand so they can manage their expectations. That way, we avoid overcrowding. Third, our supply should cope with our demand. If people leave the site disappointed because of the hassle or lack of vaccine, then they will recount their bad experience to others. But if their experience is positive, others will be motivated to be vaccinated.”
In January this year, a Pulse Asia Survey resulted in 4 out of 10 Filipinos not wanting to get vaccinated. According to Bernardo, the survey was repeated in March. This time, the figure climbed up to 6 out of 10 Filipinos refusing vaccination. “There must be something about the people’s experience in the bakuna centers that increased hesitancy—which we must address right away. Because even if the government promised a flood of vaccines eventually coming in, will people agree to be vaccinated?”
- Vaccine Hesitancy
According to DOH, 9% or over 100,000 of vaccinees who received their first dose missed out on their second dose. According to Dr. Leachon, apart from disorderly systems that discouraged Filipinos, this may be also attributed to the lack of information, leading to decreased awareness. “Maybe they don’t know where they will go to for their second dose. Different vaccine brands have different durations between the two doses. Vaccinees should be given a checklist that includes all the info they need, including when they should return.”
Leachon also suggested massive info campaigns on the possible adverse effects of the vaccine, and the mode of registration. “Online registration is very difficult for the elderly and the poor. Why should we make it hard for them? We need to have a faster registration process.” Another common complaint among registrants is the slow response of LGUs.
Recently, the issue of vaccine brands became even more heated when hundreds of Indonesian health workers became infected with COVID-19 after being fully vaccinated with Sinovac. Recently, 10 Indonesian doctors died despite their complete inoculation with the Chinese vaccine. Until now, China has not provided large-scale data on Sinovac’s effectiveness against the Delta variant. “Our life is all about choices,” Dr. Leachon said. “We choose our spouse, clothes, food. So, it’s even more important to choose what is injected into our bodies. When we don’t give people choices, we’ll have a hard time convincing them to get vaccinated.”
According to WHO, the Sinovac vaccine, in a phase 3 trial in Brazil “showed that two doses, administered at an interval of 14 days, had an efficacy of 51% against symptomatic SARS-CoV-2 infection.” With vaccine brands such as Pfizer and Moderna having an efficacy of 90% or more, some Filipinos are thinking twice about being inoculated with Sinovac. “About 70% of our vaccine inventory is Sinovac. What we’ve seen in Parañaque and Manila wherein residents flocked to the vaccination sites that gave out Pfizer is a sign that Filipinos are brand-conscious. They know their health is on the line. They value the quality, efficacy and safety of the vaccine,” Leachon said.
 “Bakuna bus”—a partnership of the Philippine Red Cross and UBE Express
“Bakuna bus”—a partnership of the Philippine Red Cross and UBE Express
Ways to improve the vaccination drive
Once the main issue of vaccine supply is addressed, our interviewees suggested the following to ramp up our vaccination drive:
- Prioritize urban areas that drive the national economy.
ABS-CBN Data Analytics Head Edson Guido recently tweeted that though COVID-19 cases in NCR are decreasing, only 7.4% of its population are fully vaccinated. Dr. Leachon suggested that prioritizing the NCR Plus Bubble can help the country achieve herd immunity faster. “We shouldn’t spread the vaccine supply thinly across the country, especially those with no cold-chain facilities. For example, we’re expecting 40 million doses of Pfizer, which will fully vaccinate 20 million people. It’s better to prioritize super metro areas like NCR Plus, which has a population of around 26 million—and 70% of that is 18 million. If herd immunity is achieved in NCR Plus, we can open our economy in time for December 2021.”
- Make vaccines more accessible.
Although mega vaccination sites may work, Dr. Leachon pointed out that these are available only in selected areas. He believes that small but multiple vaccination sites may be more efficient. “Mega vaccination sites are prone to bottlenecks and may be superspreading events. Vaccination sites should be convenient for the elderly and those with comorbidities. These sites should be many and close to residents, who can be vaccinated faster because they don’t have to worry about transportation. Because the crowd is spread out among multiple sites, waiting time is reduced.” Dr. Leachon suggested taking inspiration from successful countries, which mobilized malls, drugstores and other convenient stores which have cold-chain infrastructure in the vaccination drive.
Dr. Bernardo agreed that the solution lies in community-based vaccination sites. “We really have to bring the vaccine closer to our people, so they will be encouraged. If every barangay has a mini-vaccination site which can only accommodate 20 people a day, that can already make a big difference.” He also enjoined the government to give vaccination leaves for employees. “In bakuna centers I’ve visited, I asked those who weren’t able to get their second dose what happened. They told me it’s because they couldn’t file a leave. We have to consider living factors like this.”
To help more Filipinos be vaccinated, Red Cross Philippines has partnered with UBE Express in employing mobile vaccination buses to reach far-flung areas that do not have cold-chain facilities. “We are ready to partner with national agencies, LGUs, NGOs and private sectors to maximize this initiative and utilize all the logistical support that Red Cross could offer. When the vaccines arrive, we will go to places not accessible to health workers and NGOs.”
- Strengthen governance.
One important aspect of good governance, especially in our country, is disaster preparedness. Currently, we are in the middle of the rainy season, which may pose challenges in the vaccination drive. “First, vaccination programs are usually done in open courts, gyms and other large open spaces, which have good ventilation. But when it rains, these outdoor areas will be affected,” Dr. Leachon explained. “Second, you need to separate evacuation centers for typhoon victims, isolation and quarantine facilities, and vaccination sites. Because the moment people from these areas mix, this can be super-spreading event.” Another concern is power outages that may affect cold-chain facilities.
Government responsiveness is also important in gaining public trust and cooperation. “For example, we know that the reason why the cases are not going down is because we lack contact tracing. But the governments don’t respond to this. The same way with surveys done by SWS and DOH, which showed the participants’ preferred vaccine brands and their perceived effects. You have to execute a program based on what the citizens want, or else you will be doing the same thing all over again, but expecting a different result,” said Dr. Leachon.
 Marmick Julian, a proud vaccinee in Parañaque, displays his injected arm. (photo by Robi Robles)
Marmick Julian, a proud vaccinee in Parañaque, displays his injected arm. (photo by Robi Robles)
Achieving herd immunity
Dr. Bernardo believes that promoting vaccine confidence is an important step toward herd immunity. “The first vaccine brand we received should’ve been the best and most trusted. But a lot of doubts and issues were involved in our first vaccine—which was one of the main reasons of vaccine hesitancy.” To promote vaccine confidence, Dr. Bernardo stressed the need for better communicators. “There was a comms group that suggested that we relate vaccination to family. When you get yourself vaccinated, it’s a sign of love for your family and friends.”
As to achieving herd immunity this year, Dr. Bernardo was skeptical but hopeful. “We need 500,000 vaccinations a day if we want to have a happy Christmas this year.” Meanwhile, Dr. Leachon still emphasized the importance of vaccine efficacy. “We can only achieve herd immunity when the vaccines from Pfizer, Moderna and AstraZeneca arrive. We need to step up to the plate in the next 3 months and revisit our strategies,” he ended.
Watch Panayam sa Panahon TV’s Herd Immunity: Kailan at Paano Natin Ito Maaabot?
During the early months of the pandemic last year, the demand for ginger surged all over the world. But due to the virus, import shipments of goods including ginger were delayed. Because the supply could not meet the demand, ginger prices drastically rose in many countries. According to this article, these include Ethiopia, wherein the “wonder root” was sold almost three times more than its original price.
The focused interest in ginger came when global health authorities were still churning out initial information on COVID-19. At the same time, social media blazed with claims of ginger being a COVID-19 cure. This prompted the World Health Organization (WHO) to nullify such claims, stating that “There is no scientific evidence that black pepper, honey and ginger protect from COVID-19 infection. In general, however, some spices are considered to have properties that may be beneficial for health.”
The National Academies of Sciences, Engineering and Medicine goes further by saying that
“Viral infections spread in your body when the virus enters your cells and makes copies of itself and then those copies enter new cells and repeat the process. Ginger will not destroy the virus in your body or stop the copying process.”
This article stated that during a press briefing, Executive Director of WHO Health Emergencies Program Michael Ryan acknowledged that herbal teas such as ginger are beneficial. Still, he warned against false statements that may lead to pandemic risks. “Anything that makes one feel better, anything that provides that reassurance and anything that you believe can help your health that’s not dangerous certainly has a positive impact on your health, but it’s a different thing to say that something is effective in treating the disease,” he said.

Powers of Ginger
For centuries, ginger has been an important part of Filipino cuisine and folk medicine. This comes as no surprise because ginger originated in Maritime Southeast Asia, which includes the Philippines. During the spice trade in 1500 BC, ginger even reached Europe and was used by ancient Greeks and Romans.
Ginger is a popular ingredient of our local dishes such as tinola, arroz caldo and pinakbet, and is known to effectively eliminate fishy odors in seafood-based recipes. But when it comes to home remedies for colds and sore throat, one of the most popular is salabat, traditionally made from boiled fresh ginger.
In a Panahon TV interview with Gab Labrador, a nutrition officer at the National Nutrition Council, he explained in a mix of Filipino and English that ginger became popular during the pandemic because “it helps reduce inflammation brought by respiratory diseases.” In fact, a 2008 study by the Common Cold Center at the Cardiff University in Wales concluded that hot drinks like salabat can soothe “runny nose, cough, sneezing, sore throat, chills and fatigue” better than beverages in room temperature.
Labrador also shared ginger’s other health benefits:
- Has a good amount of fiber that’s good for digestive health
- Can calm an upset stomach and acts as a laxative
- Alleviates dizziness and nausea
- Is high in antioxidants that reduce cell damage
- Boosts immune system
- Reduces the risk of heart disease
- Controls blood sugar levels
But is there such a thing as ingesting too much ginger? Labrador said that though the effects of eating excess ginger are rare, they are still possible. “It can lead to an upset stomach and heart burn. There may be some people who are allergic to spices like ginger. The allergy manifests through skin inflammation.” He also added that ginger may interact with some drugs. “These are the anticoagulants or blood thinners. If you’re taking these drugs, you might want to ask your doctor if you can still take ginger tea.” To avoid complications, Labrador recommended limiting the salabat we drink to one cup a day.

Staying Healthy During the Pandemic and Beyond
Though ginger is undoubtedly beneficial to our bodies, staying healthy this pandemic is still all about avoiding exposure to the virus. “That’s basically following health protocols— social distancing, proper hygiene…and it’s better for the population to take the vaccine once it’s offered to them,” said Labrador.
Echoing WHO, Labrador is all for taking salabat if it makes people feel better. But he warned, “It’s not really good to brand natural remedy as a cure of a certain disease. So, it’s still better to get proper medical action from a medical professional during these times.” Moreover, we can strengthen our immune system by having a holistic approach toward health “Number one is to eat a variety of foods including fruits and vegetables every day. Prioritize natural and fresh foods over highly-processed or fast food. We also want to maintain a physically active lifestyle during these times. Just go to the internet and search for body weight exercises that you can do. That can definitely help us in improving our immune system and maintain a healthy weight which…in the long run, will benefit us.”

How to Prepare Salabat
Labrador gives these steps in preparing your own throat-soothing ginger tea:
- Thinly slice ginger into 5-6 pieces.
- Boil them in a cup of water.
- Boiling time depends on how strong you want the ginger flavor to be. 10 minutes will result in a mild ginger taste, while 15-20 minutes will bring out the ginger’s spiciness.
Watch our interview with Gab Labrador here.
A year after the pandemic, the World Health Organization updated its health advisory last April, stating that COVID-19 may be acquired through airborne transmission. This is in addition to the droplet transmission, which was previously the widely recognized mode of spreading the virus.
But what does this new discovery entail? Panahon TV sought the advice of Dr. Rontgene Solante, chairman of the Adult Infectious Diseases and Tropical Medicine Department at the San Lazaro Hospital, and a member of the Vaccine Expert Panel of the Department of Science and Technology.
Droplet vs Airborne Transmission
Dr. Solante mentioned that the COVID-19 virus is expelled through coughing, sneezing, or talking. The Centers for Disease Control and Prevention (CDC) adds to this list by stating that “People release respiratory fluids during exhalation (e.g., quiet breathing, speaking, singing, exercise, coughing, sneezing) in the form of droplets across a spectrum of sizes. These droplets carry virus and transmit infection.”
“The droplet is composed of virus particles within the saliva,” explained Dr. Solante in a mix of English and Filipino. “This means it’s much bigger and heavier. When you cough or sneeze, the droplet can travel up to 3 feet. It falls quickly on surfaces.” It’s because of these reasons why COVID-19 prevention involves regular hand washing and regularly disinfecting frequently-touched surfaces.
On the other hand, COVID 19’s airborne transmission involves the aerosolized form of the virus. “Why is it aerosolized? It’s because when you cough, you expel not just droplets but also tinier particles. These particles are lighter so they stay in the air longer. This is what we call airborne.”
While droplets are most infectious within a 3-feet or 1-meter distance between people, the airborne particles, which can remain suspended in the air for up to two to three hours, may infect people within an 8-feet distance.
According to the World Health Organization (WHO), medical procedures and treatments that produce aerosols may also transmit COVID-19. These include endotracheal intubation, open suctioning, administration of nebulized treatment, manual ventilation before intubation, turning the patient to the prone position, and disconnecting the patient from the ventilator.
The CDC states that the higher the amount of virus a person is exposed to, the higher the risk of infection. Through the airborne transmission, you are more likely to catch COVID-19 when the following factors are present:
- Enclosed spaces with poor ventilation. This includes air-conditioned spaces that let droplets and aerosol particles build up in the air.
- Increased exhalation of an infected person’s respiratory fluids. This person doesn’t need to cough or sneeze to spread the virus. He or she may simply be shouting, singing or engaged in a form of physical exertion such as an exercise.
- Prolonged exposure to these conditions for more than 15 minutes.
 Though bikers are required to wear face masks, they do not have to wear face shields as these pose safety risks according to the Department of Health. (photo by Jire Carreon)
Though bikers are required to wear face masks, they do not have to wear face shields as these pose safety risks according to the Department of Health. (photo by Jire Carreon)
What Airborne Means
“Airborne diseases are easily transmitted when you are not wearing the proper face mask, when ventilation is very poor, and more importantly, when you are in a closed space,” warned Dr. Solante. Tuberculosis is an example of an airborne disease. “The reason why the Philippines has a high case of Tuberculosis is because many of us live in communities with houses built close to each other. When one has this disease, he or she is likely to transmit it to family members. In a way, this is similar to COVID-19, which easily spreads within the household because of the droplet and airborne modes of transmission.”
The fact that COVID-19 is airborne and may be transmitted beyond 6 feet only means that more than ever, we need to be vigilant about health protocols, and stay in well-ventilated areas. Dr. Solante said, “Chances are, if you are in a room without ventilation or with poor ventilation, the virus can stay longer— for about 3 hours. The minute you remove your face mask or face shield, then you can get the virus within 15 minutes of staying in that closed space.”
But what does proper ventilation mean? Dr. Solante said this is achieved when air inside the room is able to flow out, while air outside the room is able to flow in. “Without air ventilation, the aerosolized virus can stay in the air for two to three hours. But if you open the windows, and there’s ventilation, the virus will only be airborne for less than 15 or 30 minutes, as long as there are only a few people inside the room.”
 Sign inside a jeepney. This year, face shields were also required inside public transportation. (photo by Paul Michael Caisip)
Sign inside a jeepney. This year, face shields were also required inside public transportation. (photo by Paul Michael Caisip)
How to Prevent Airborne Transmission of COVID-19
Dr. Solante offers these prevention tips in various settings:
At home
- Open windows to encourage ventilation.
- If the heat is too much, and you want to turn on the air-conditioning, make sure to have less conversations and interaction among family members inside the room. Wear face masks, and limit the number of room occupants.
In the office
- Maintain a distance of at least six feet from other people.
- Limit the number of people in the room.
- Always wear your face mask and face shield inside the room. Dr. Solante doesn’t recommend doubling your masks as this may make breathing difficult.
- Avoid unnecessary talking. Use chats or other forms of communication that don’t require you to open your mouth.
- Always practice cough etiquette and regular hand washing.
- If ventilation is poor in the office, Dr. Solante urges the management to consult with engineers on how to improve air flow.
In Public Transport
- Always wear a face mask and face shield. Make sure your eyes, nose and mouth are covered.
- Try not to open your mouth. This means avoiding activities such as eating, conversing and talking on cellphones.
- Maintain physical distancing. Passengers should at least be a seat apart.
In a nutshell, Dr. Solante gives these 5 important tips during the pandemic:
- Practice regular hand washing.
- Wear your face mask and face shield.
- Maintain a physical distance of six feet or more.
- Avoid crowded areas.
- Only visit places with good ventilation.
Though the airborne transmission is cause for alarm, following health protocols is still an effective countermeasure. Complying to guidelines set by health experts and being vaccinated are still your best bets in safeguarding your health and that of other people.
*interview by Trisha Garin
Watch Panahon TV’s interview with Dr. Solante here.
In a recent public address, Vaccine Czar Carlito Galvez stated that over 3 million Filipinos have been vaccinated since March 1, 2021. But it is still a far cry from the 70 million the government targets to vaccinate by the end of this year to achieve herd immunity.
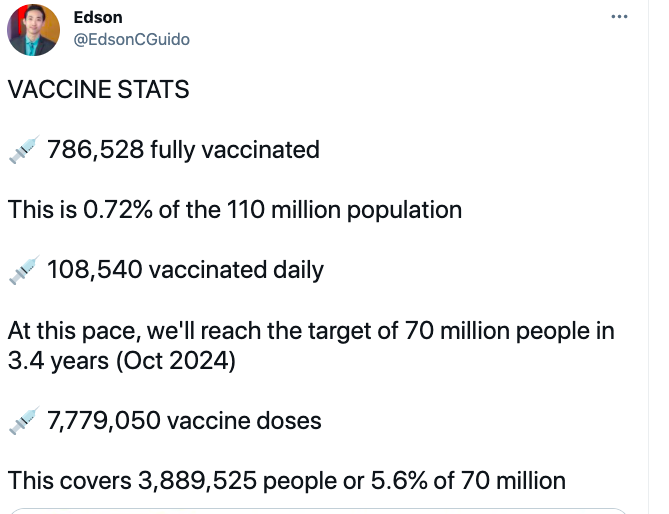
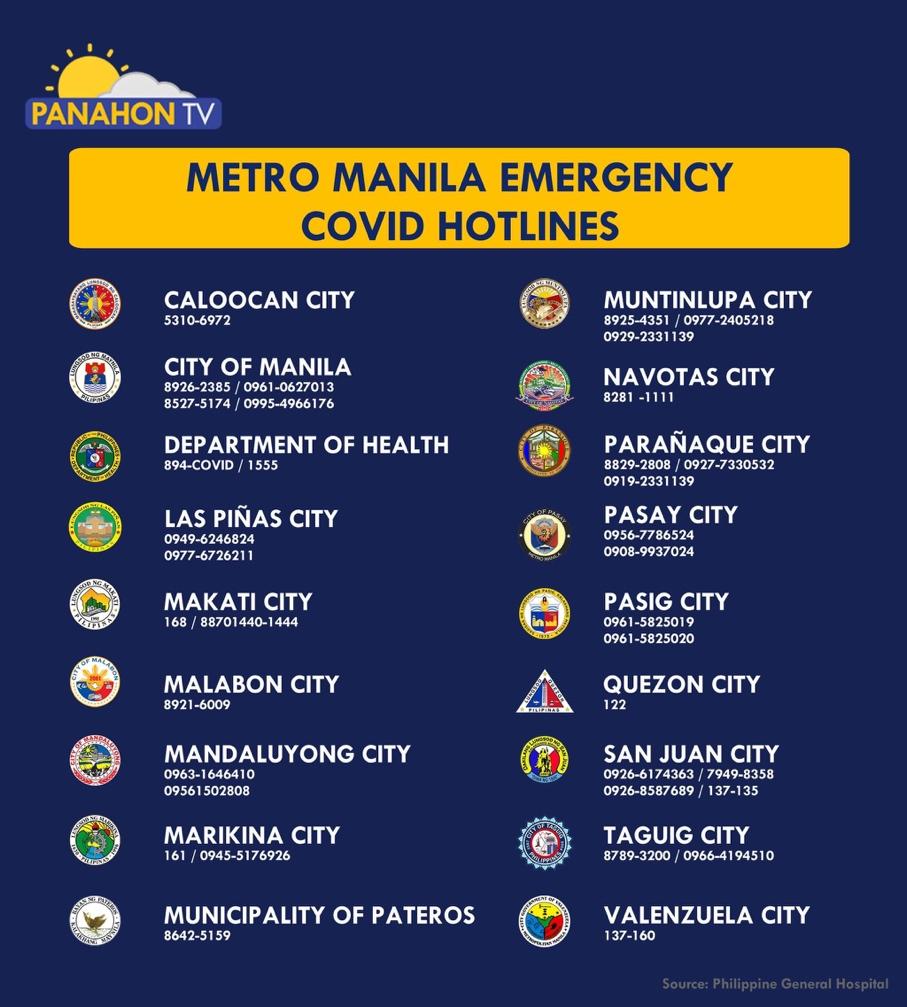
The Department of Health (DOH) stated its plans to inoculate 100,000 to 200,000 individuals daily once vaccine supplies become stable. But from the 7 million vaccine doses received by the country so far, over 3 million have only been administered nationwide. A tweet from ABS-CBN Data Analytics Head Edson Guido two days ago (May 19, 2021) further brought to light how far the country is from herd immunity. He stated that at the rate we are going, the 70-million target will be achieved in 3 years, and not this year. “We still have a long way to go,” Guido tweeted. “To reach the target of 70 million by end of 2021, the average should be around 600,000 daily. That’s 5.5 times the current pace. We need more vaccines.”
 (screenshot from Twitter)
(screenshot from Twitter)
Adding to the challenges of vaccine supply and vaccination processes is the sensitivity of some vaccine brands. To ensure their safety and efficacy, they need to be maintained in very low temperatures in every step of the way— from their arrival in the airport to storage and delivery. With the country’s limited infrastructure especially in remote areas, vaccine quality may suffer, and along with it, the health of many Filipinos.
 Fr. Nic in the Providence College laboratory (Courtesy: Providence College)
Fr. Nic in the Providence College laboratory (Courtesy: Providence College)
Developing a Different COVID-19 Vaccine
Such issues are what a new type of COVID-19 vaccine hopes to resolve. Fr. Nicanor “Nic” Austriaco, who is developing this product, has taken his cue from oral vaccines such as the one for polio. “It’s not unusual to have oral vaccines,” he explained. “In the Philippines, we have 110 million people in 7,000 islands, and we have to bring the vaccine to them. Right now, all the (COVID-19) vaccines require very cold refrigerators. I want to develop a vaccine that is shelf-stable. In other words, you can put it on the shelf without the need for refrigeration, and it would still last.”
Biology and theology are Fr. Nic’s fields of expertise, having been trained in molecular biology at the Massachusetts Institute Technology (MIT) in the U.S. more than two decades ago. Currently, he is a professor at both the Providence College in Rhode Island and our very own University of Santo Tomas. He is also a fellow at OCTA Research, an independent and interdisciplinary research group of faculty members that has been providing pandemic data for the country.
The vaccine Fr. Nic and his team are developing is yeast-based, with a shelf life of two years even without refrigeration. “The idea is that we take probiotic yeast, which you can buy in drugstores, and we genetically engineered it. We changed it so that it will produce the spike protein of the SARS-CoV-2 virus. This spike protein is the part of the virus that Pfizer, Moderna , AstraZeneca, Gamaleya all put into your body. So, we are just changing the delivery system.” The yeast, which could be drunk or taken in pill form, would stay in the intestines and produce the spike protein, which would trigger the body’s immune system.
Despite the promising benefits of this oral COVID-19 vaccine, Fr. Nic warned that it may take 6 months to a year before it can be released to the public. “This is why I call this a second- generation vaccine. The expectation is we’re going to be vaccinated nearly every year or nearly every other year. So to save the Philippine government [from spending] billions of pesos to be paid every year to foreign companies, we’re trying to develop a vaccine for the Philippines that is relatively cheap but safe and efficacious.”
Fr. Nic named the oral vaccine development as Project Pag-asa, precisely because he hopes to give hope to Filipinos, especially the poor. “I read a story about a Filipino jeepney driver who lost his job, who lost his house because of the first ECQ, and I realized that we have to protect the poor—the poorest kababayans. The first-generation ones will be great for them but if we do this every year for a long time, we need a vaccine that would be easily accessible to our poor kababayans.”
Like other vaccine developers, Fr. Nic’s team is developing two versions of the oral vaccine—one for the original COVID-19 strain, and one for the other variants. Regarding questions on the oral vaccine dosage, Fr. Nic said that it would depend on the clinical trial. Once the yeast is developed, the first step is to do animal testing. “Once the animal testing is done— if that is successful— then we have to go to clinical trials in the Philippines. So, there are still many steps that we need to do before we can make it available to the public.”
 Developing the COVID-19 oral vaccine (Courtesy: Providence College)
Developing the COVID-19 oral vaccine (Courtesy: Providence College)
Importance of Vaccination
Fr. Nic has already been vaccinated with the Moderna vaccine in the States. He was part of the priority list because he resided in a community of priests, which had elderly members. “The side effects can be rough, especially after the second dose. I was very sick for about one day. I had headache, body ache, fatigue, chills for many hours. But after that day, it was gone.”
Still, Fr. Nic reiterated that the sick feeling after vaccination is a sign that the vaccine is working. “It’s your body fighting the vaccine already. That is why the second dose is worse than the first dose. The older you are, the easier the side effects, If you are young, you can be really, really, really sick because you have a stronger immune system. So, the immune system fights back stronger and you feel sick more— but only for one day. And if you had COVID before, especially if you didn’t know you had COVID, the first dose would be harder than the second dose.”
As for those hesitating to get vaccinated, Fr. Nic said, “I’m one of them who have been vaccinated against COVID-19. I can now walk around the city. I can get on a plane. I can visit other people. It is the quickest way to end the pandemic, right? I am sure you are tired of ECQ. You are tired of lockdown. The only way we can stop this is if all the Filipino adults—70 million adults choose to be vaccinated.”
For Fr. Nic, vaccination is not only a self-protective measure, but also a caring decision.
“Why do we get vaccinated? We get vaccinated to protect ourselves, but more importantly, to protect those around us who are more vulnerable to the disease. When I was being injected by the second dose, I thought ah, my mom is safe now. I was so concerned about my mother’s well-being. She’s a senior citizen, so every time I visit her [in Manila], I was worried that I would secretly bring the virus to her. Now, I know she is safe because I am vaccinated. We are vaccinated not only to protect ourselves but also to protect our parents and our grandparents. Those are really important to understand, especially in the Philippines.”
* interview by Blueberrie Recto
Watch Panahon TV’s interview with Fr. Nic here.
Sometimes, it only takes a small step to spark a movement.
When 26-year-old Ana Patricia “Patreng” Non decided to start a community pantry near her home in Maginhawa Street, Quezon City, it was because she wanted to help. “My small business was affected because of the lockdown,” she explained in Filipino in a Panahon TV interview. “But even if I didn’t have any income, I could still eat three times a day. I thought of those whose livelihoods depended on being out on the streets. They needed support.”
Soon, news about Patreng’s Maginhawa Community Pantry, fashioned from a bamboo cart, spread like wildfire. People came in droves, dropping off food donations, and getting food. The initiative was so popular that even the German Ambassador to the Philippines Anke Reiffenstuel dropped by to donate goods. She tweeted that she was “deeply impressed by the solidary spirit of the Filipinos.”
 Patreng and her bamboo cart of donated goods (photo from AP Non)
Patreng and her bamboo cart of donated goods (photo from AP Non)
Maginhawa Community Pantry’s Evolution
To accommodate the growing volume of crowd and donations, the pantry relocated to a bigger space at the Teacher’s Village East Barangay Hall. Quezon City authorities were called in to maintain health protocols. But the line continued to grow, extending all the way to Philcoa along Commonwealth Avenue. Senior citizens, though prohibited to go out of their homes, joined the queue. To get in line early, people broke curfew.
To address these challenges and to meet the needs of community pantries that mushroomed in the area and all over the country (as far as Mindanao), the Maginhawa Community Pantry recently announced that it would no longer serve beneficiaries. Instead, the pantry has evolved into a drop-off point for donations, which will be distributed among other pantries and places that needed aid. This decentralizing move seeks to promote better barangay coordination and observation of health protocols, and to spread out the crowd lining up for goods.
 Inspired by Patreng’s initiative, UP Campus residents set up their own community pantry. (photo by Mary Jhoy Aap)
Inspired by Patreng’s initiative, UP Campus residents set up their own community pantry. (photo by Mary Jhoy Aap)
Ensuring Safety in Community Pantries
Though initiating community pantries is commendable, organizers should always remember that the country is still grappling with the pandemic. Safety and Preparedness Advocate Martin Aguda Jr. explained in Filipino, “Each time you go out—whether you’re an organizer, a volunteer, a donor or a beneficiary—you are at risk for COVID-19, especially in crowded community pantries.”
On the day when a senior citizen collapsed and died while waiting in line at a community pantry, the Quezon City government released its Community Pantry Guidelines to minimize health risks. Aguda also offers these tips:
Map out a risk management plan. Recognize the risks of your endeavor. How will these affect everyone involved? “You have to check the risks and you have to put in your safety measures,” stressed Aguda. The risk management plan involves wisely choosing the pantry’s location, which will largely depend on the crowd volume you are capable of handling. “Is this an area that will draw in crowds? You need to survey the place because from there, you can gauge your expected crowd.”
Check if your resources are enough. Make sure that the amount of goods you will be distributing matches the expected number of beneficiaries. “When the people outnumber the goods, that will result in long lines and extended waiting time. The longer people wait in line, the more they are exposed to other people and the risk of COVID,” shared Aguda. Limited resources may also cause people to forego discipline and cause a stampede.
Ensure the safety of everyone involved. Aside from making sure everyone is wearing a mask and a face shield, and is practicing physical distancing, organizers should also check the pantry’s surroundings. Aguda explains, “The location should be away from traffic to prevent accidents. Physical distancing can be enforced through physical markers. Enlist the help of safety officers or barangay officials to ensure that lines and health protocols are followed.” Aguda also suggested to set early operation hours so people don’t have to wait under the heat of the sun. This reduces the risk of heat stroke and dehydration.
Regularly brief the crowd. Reminding the crowd to follow health protocols cannot be made often enough. Because there’s always a fresh batch of people joining the line, always reiterate the measures to ensure their safety. Set an example by wearing PPEs and following physical distancing. Provide alcohol for public use.
“It all boils down to planning. We all want to help, but we don’t want to deal with unintended consequences,” warned Aguda. He advised people going to community pantries to also bring drinking water and umbrellas. “Learn to be practical. Remember your health is at risk.”
In turn, Aguda advised organizers to never let their guards down. “You need to protect yourself because you are interacting with different people. Don’t remove your mask at any time. Your volunteerism is a noble act, but you can still help others by ensuring your own safety,” he ended.
Watch Panahon TV’s full interview with Martin Aguda Jr. here.
For those who want to donate to the Maginhawa Community Pantry, visit its Facebook page.
Only a week to go before the end of April when the government will decide whether to change or maintain the current MECQ (Modified Enhanced Community Quarantine) status in NCR Plus. But with the Department of Health’s report on having 66% of the country’s ICU beds solely for COVID-19 patients already utilized, it is clear that the healthcare system still needs more time to recover. In fact, PGH (Philippine General Hospital) spokesperson Dr. Jonas del Rosario stated, “Extension of MECQ will probably help in further decreasing the transmission, and then fewer people will get hospitalized.”
As of writing, the World Health Organization (WHO) has recorded over 143 million confirmed cases of COVID-19, and over 3 million deaths worldwide. Because this scenario may be difficult to imagine, Dr. Anna Lisa Ong-Lim, division chief of the Department of Pediatrics’ Infectious and Tropical Disease in PGH offers this explanation: “That means every man, woman and child who lives in the Philippines has tested positive. When you talk about the deaths, that’s kind of saying that everybody in Quezon City has died of COVID.” She added that she wouldn’t be surprised if the DOH’s current tally of over 971,000 cases hit 1 million very soon. As of April 22, the country’s total active cases are almost 108,000 with over 16,000 deaths.
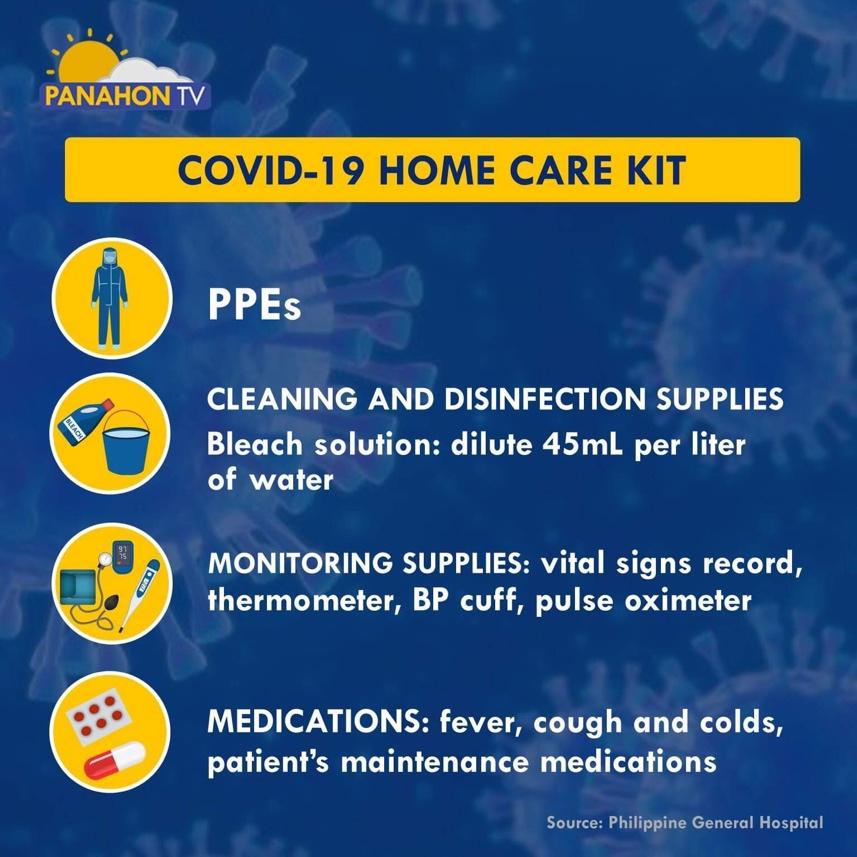
With NCR hospitals in almost-full capacity, alarming stories of patients having to go outside of Metro Manila to seek medical care abound. But with DOH stating that more than 97% of current COVID-19 cases are mild and asymptomatic, home care may be feasible. To learn more about this, The Sanctuario de San Antonio Parish Team held the webinar entitled What to Do When COVID Hits Home with Dr. Ong-Lim as guest speaker.
When COVID Homecare is Feasible
In March last year, WHO began releasing homecare guidelines for mild cases when “in-patient care is unavailable or unsafe”, which is currently the case in NCR. To determine which cases are eligible for home care, Dr. Ong-Lim proposes asking three questions:
- DOES THE PATIENT QUALIFY FOR HOME CARE?
According to WHO, the following cases qualify for home care:
- Asymptomatic or those with mild or moderate disease
- No risk factors for poor outcome. Risk factors include being more than 60 years old, smoking, obesity, cardiovascular disease, diabetes, chronic lung or kidney disease, immunosuppression and cancer.
Dr. Ong-Lim expounds on this by saying that the patient should not have difficulty in breathing to qualify for home care. This can be concluded when the patient is able to do the following:
- Comfortably breathe and does not have any shortness of breath
- Comfortably speak in full sentences. Patient doesn’t catch his/her breath when speaking.
- Has a respiratory rate of less than 30 breaths per minute at rest
- Oxygen saturation without any oxygen supplementation is at least 94%. This can be measured by using a pulse oximeter device.
- IS THE HOME SETTING SUITABLE FOR HOME CARE?
Though both isolation and quarantine seek to limit the patient’s movement to avoid passing on the virus, Dr. Ong-Lim enumerated their differences.
| ISOLATION | QUARANTINE |
| For someone who tested positive for COVID-19 | For someone who had been in close contact with a positive case |
| Duration is about 10 days | Duration is 14 days
|
| Patient should have no fever or symptoms for at least 3 days before he/she is discharged from isolation. | Quarantined person should watch out for symptoms, check temperatures, and avoid contact with others, especially those at high risk. |
Physical requirements for home care include:
- A separate room and bathroom for patient. Patient’s door need to be closed to contain airflow.
- A delivery system for patient’s daily needs that allow minimal exposure for caregiver.
- Only one caregiver for patient. Caregiver should be in good health without underlying chronic conditions.
- If contact and exposure with patient is necessary, caregiver should wear a face shield and face mask, and maintain a distance of 1 meter from the infected person.
Additional tips for infection prevention in the home include:
- Provide patient with medical masks. After use, masks should be disposed of in a separate trash bin.
- Patient should have his/her own utensils and linen. Before washing used linen, place them in a laundry bag. Don’t shake the bag so as not to aerosolize the virus. Use regular soap and water for washing. Wear gloves and a face mask when washing.
- Frequently clean and disinfect surfaces at home. Wear gloves and a face mask when cleaning. A disinfecting solution consists of 45 ml bleach for every liter of water. Prepare the solution daily because this evaporates, affecting its efficacy.
- If patient used a shared space such as the bathroom or kitchen, sanitize the area right away.
- Household members should constantly practice hand hygiene.
- Visitors should not be allowed in the home.
- CAN THE PATIENT BE PROPERLY MONITORED AT HOME?
Aside from having no risk factors and being below 60 years old, the caregiver should also also be reliable. This ensures the accuracy of information that will be relayed to the healthcare professional.
According to Dr. Ong-Lim, the caregiver should be equipped to do the following:
- Monitor vital signs of patient by recording the date, time, heart rate, respiratory rate, oxygen saturation, temperature and blood pressure. Do this 1 to 3 times, or every 8 hours daily.
- Make sure patient takes his/her maintenance medicines.
- Maintain a supply of medication for fever, cough, and colds.
- Be vigilant of worsening symptoms that require urgent professional care.
The Centers for Disease Control and Prevention (CDC) states that these signs merit emergency medical attention:
- Trouble breathing
- Persistent pain or pressure in chest
- Patient being confused and disoriented, which may be a sign of decreasing oxygen levels in the body
- Inability to wake or stay awake
- Pale, bluish gray skin, lips or nail beds
Dr. Ong-Lim added that patients with mild to moderate disease without risk factors could take about 10 days to recover. The important thing is that the patient should be improving, and not progressing toward severe or critical illness. When the latter happens, the patient needs to be transferred to a hospital.
A Side Note on Ivermectin
So far, three hospitals in the country have secured permission to use ivermectin against COVID-19. Oral ivermectin, which was previously used in the Philippines only for parasite infestations among animals, is now allowed by the Food and Drug Authority (FDA), under a special permission, to be given to COVID patients. Currently, ivermectin clinical trials in the country are underway.
However, health experts including the FDA and WHO have been vocal against the use of the drug, citing that there isn’t enough evidence to prove that its effectivity against COVID-19. About this, Dr. Ong-Lim said, “Even if there are scientific publications saying that there is evidence for it, unfortunately, the studies are affected by the fact that they involved different kinds of populations. Ivermectin in those trials may have been used with other interventions, so it’s very difficult to isolate and say that the effect is solely due to ivermectin.”
Aside from its lack of efficacy, health experts are also concerned about ivermectin’s possible toxicity. “Is it right to put our faith into something that needs more sound evidence?” Dr. Ong-Lim asked in Filipino. “We need more evidence before we can trust it. Otherwise, we have misplaced faith. We need to understand what we’re really afraid of. We’re afraid of getting sick. How can we prevent that? By just utilizing your mask and shield properly, your distancing, your circulation, and your time of interaction— if you put that all together, the numbers supporting prevention with the proper use of your PPEs is much, much higher than any intervention, whether that’s ivermectin or even some of the vaccines.”
Watch the full webinar here.
As the Philippines continues its COVID-19 vaccination drive, its active cases have spiked past 86,000, including the country’s highest single-day increase since the pandemic began. A year after lockdown was declared, the health system is, once again, overwhelmed.
While the Department of Health’s hospital referral system is swamped with calls about new cases, 30 hospitals in NCR have declared full bed capacities for COVID-19 patients. COVID-19 variants have been detected in all cities in Metro Manila, prompting the government to place the area as well as Cavite, Laguna, Rizal and Bulacan in a bubble from March 22 to April 4. Within this period, only essential travel will be allowed into and out of these places.
More than ever, faster and more efficient processes need to be in place, especially since only over 500,000 have so far been inoculated—less than 1% of the 70 million targeted to achieve herd immunity this year. To better understand this issue, we discuss key points of an online discussion held by the Women’s Business Council of the Philippines, featuring health-sector heavyweights such as Former Health Secretary Dr. Esperanza Cabral; Dr. Susan Pineda-Mercado, director of Food Systems and Resiliency at the Hawaii Institute for Public; and Dr. Tony Leachon, chairman of Kilusang Kontra-COVID.
 The Parañaque government began its vaccination of senior citizens last March 22, 2019
The Parañaque government began its vaccination of senior citizens last March 22, 2019
The Need for Vaccines
In the online talk held last February, Dr. Cabral expressed her pro-vaccination views, stating how the Centers for Disease Control and Prevention (CDC) listed vaccination as one of the 10 greatest public health achievements of the 21st century. “Vaccines have gone to develop into the most life-saving medical advancement in history,” she said.
Meanwhile, Dr. Mercado explained how the COVID-19 vaccination could protect one’s health. “You get a tiny bit of the virus, and that will stimulate the development of the antibodies. It helps you recognize the enemy because if you get natural exposure, your disease will not be moderate or even severe.”
With mass vaccination enabling majority of the population to develop a considerable degree of immunity against COVID-19, Dr. Cabral stated the following possible benefits:
- Protects us, our loved ones and communities from disease and death
- Enables us to reopen our society
- Prevents our health care workers from being overwhelmed
- Frees us up to address the non-COVID diseases we suffer from
“Why are vaccines important to us? They are important to us because if there is a vaccine for a disease, it will prevent that severe disease and death from it,” Dr. Cabral said. “It will prevent symptomatic disease and importantly, it will also prevent the transmission of disease to others.”
 Dr. Grace Pagayon-Uy received her first jab of AstraZeneca as part of the QC government’s vaccine rollout for health care workers this week.
Dr. Grace Pagayon-Uy received her first jab of AstraZeneca as part of the QC government’s vaccine rollout for health care workers this week.
The Importance of Starting Early
But as Dr. Mercado stated, mass vaccination does not guarantee an immediate victory against the virus. The changes are likely to be felt gradually, which is why early intervention is key. Dr. Cabral enumerated these results of Israel’s early vaccination drive, which started in January:
- COVID-19 vaccine was 98.9% effective in preventing deaths and hospitalizations.
- COVID-19 vaccine was 98% effective in preventing infections that prompted fever or breathing problems.
- Infection rate declined by 95.8% among those who received two doses of the vaccine.
To guarantee early vaccination, Dr. Leachon shared that acquisition of vaccines should start as early as the phase 2 of clinical trials—which is what Vietnam, China, India and South Korea did. He presented a projection of good economic growth among these countries. Meanwhile, poor pandemic response resulted in the plummeting economies of the US, Brazil and the UK.
 AstraZeneca vaccine arrive in the Philippines from the COVAX facility last March 4. (Photo from National Task Force Against COVID-19)
AstraZeneca vaccine arrive in the Philippines from the COVAX facility last March 4. (Photo from National Task Force Against COVID-19)
On the Flip Side: Anti-Vaxxers
The World Health Organization included “vaccine hesitancy” in one of the top global health threats in 2019. WHO stated, “Vaccine hesitancy – the reluctance or refusal to vaccinate despite the availability of vaccines – threatens to reverse progress made in tackling vaccine-preventable diseases. Vaccination is one of the most cost-effective ways of avoiding disease – it currently prevents 2-3 million deaths a year, and a further 1.5 million could be avoided if global coverage of vaccinations improved.”
WHO identified the possible reasons for vaccine refusal:
- Complacency
- Inconvenience in accessing vaccines
- Mistrust or lack of confidence
Throughout history, anti-vaxxers—the term used for those who oppose vaccines—have cited various side-effects from vaccines. These included infertility, brain damage, and most recently, autism, which some claimed were an effect of the MMR (measles, mumps and rubella) vaccine for children. This resulted in a decline in MMR vaccinations, which, in turn, resulted in an emergence of measles and mumps in Europe and North America, which had not seen these diseases for many years. According to the CDC, studies have dispelled the claim linking vaccinations to autism.
 Dr. Gladys Lacuna-Mendoza gets her first dose of Sinovac vaccine. According to Sec. Carlito Galvez, chief implementer of the National Task Force Against COVID-19, almost 24% of the country’s 1.7 million health workers have been vaccinated.
Dr. Gladys Lacuna-Mendoza gets her first dose of Sinovac vaccine. According to Sec. Carlito Galvez, chief implementer of the National Task Force Against COVID-19, almost 24% of the country’s 1.7 million health workers have been vaccinated.
Convincing the Skeptics
A recent survey from OCTA Research revealed that 46% of Filipinos are unwilling to get inoculated against COVID-19 even if the vaccine was proven safe and effective. To combat this massive vaccine hesitancy, Dr. Cabral urged the government to use “trustworthy and trusted talking heads, and use language that people can easily understand.” Messages should also be balanced and consistent, and widely reiterated across all platforms.
Dr. Leachon even warned that future travel might require COVID-19 immunity passports. “This is important to economic recovery and that’s why we need to have vaccination. The Philippines will be isolated from the rest of the world if we will not be vaccinated— tourists will hesitate to come, the international business people will not travel, Filipinos may not be given passes to travel abroad, thus curtailing business activities and even family leisure and travel. Our competitiveness will sink even further in the rankings.”
But even with vaccination, Leachon said health measures should still be improved such as contact tracing, quarantine and isolation facilities, and even government messaging. “We should invest in health care so we can prepare for the next pandemic. We have to take better care of our health care workers.”
Still, even if public acceptance of vaccination improves, the slow arrival and rollout of COVID-19 vaccines remain a major hindrance. All the health experts in the online discussion agreed that right now, there is no room for complacency. To save lives and the economy, vaccination needs to be a priority. “The economy will never recover as long as the virus is not controlled. And if you don’t understand that, then we’re part of the problem,” ended Dr. Leachon.
Donna May Lina at Agay Llanera
Dahil buong mundo ay abala sa pagpuksa ng COVID-19, laging laman ng balita ang pagpapabakuna laban sa sakit na ito. Ayon sa Bloomberg, ang Estados Unidos ang nangunguna sa dami ng mga nabakunahan. Pumapalo sa halos 2.5 milyon ang natuturukan ng COVID-19 vaccine sa U.S. kada araw.
Simula nang inumpisahan ng Pilipinas ang vaccination drive nito n’ung March 1, higit sa 240,000 ang nabakunahan nang mga Pilipino. Ngunit bukod sa mabagal na pagdating ng mga vaccine, hadlang sa malawakang vaccination ang kawalan ng tiwala ng mga Pilipino sa vaccine. Ayon sa isang survey, 46% ng mga Pilipino ay hindi papayag mabigyan ng COVID-19 vaccine kahit na napatunayan itong ligtas at epektibo.
Kasaysayan ng Bakuna
Pinaniniwalaan na ang English physician na si Edward Jenner ang unang nagsagawa ng matagumpay na pagpapabakuna. Pagkatapos niyang turukan ng smallpox virus ang isang bata, nagkaroong ang pasyente ng immunity sa nasabing sakit. Nang nagkaroon na ng mass vaccination, tuluyan nang naiwaksi mula sa mundo ang small pox noong 1979.
Ayon sa Centers for Disease Control and Prevention (CDC), mahalaga ang childhood vaccines o ‘yung mga bakunang ibinibigay sa mga sanggol at bata sa pag-iwas sa sumusunod na mga sakit:
- polio
- tigdas (measles)
- diphtheria
- pertussis (whooping cough)
- tigdas-hangin (German measles)
- beke (mumps)
- tetanus
- rotavirus
- Haemophilus influenzae type b (Hib)
Ang mga bakuna ay nagbibigay proteksyon, hindi lang sa indibiduwal, kungdi pati rin sa buong komunidad.
Ano ang Herd Immunity?
Inilalarawan ng World Health Organization (WHO) ang herd immunity bilang indirektang proteksyon laban sa isang nakahahawang sakit. Maaaring magkaroon ng immunity ang isang populasyon mula sa pagpapabakuna o dati nang pagkakasakit. Dahil posibleng mabiktima ng COVID-19 nang higit sa isang beses, inirerekomenda ng WHO ang pagpapabakuna laban dito upang makamit ang herd immunity.
Para hindi dapuan ng matinding COVID-19 ang malaking bahagi ng populasyon, isinasagawa ng mga bansa ang malawakang vaccination. Herd immunity rin ang layunin ng pamahalaan ng Pilipinas kaya inanunsyo nito ang planong mabakunahan ang 70 milyong Pilipino sa loob ng isang taon.
COVID-19 Vaccination Plan sa Pilipinas
Noong Pebrero, inilabas ng Inter-Agency Task Force for the Management of Emerging Infectious Diseases (IATF-EID) ang priority list o ‘yung pagkakahanay ng mga mababakunahan.
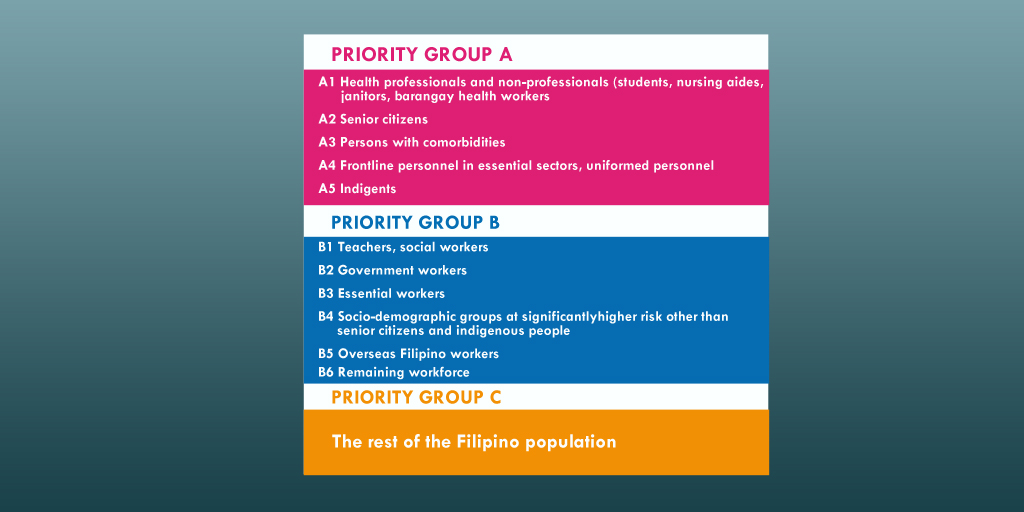 Source: Philippine News Agency (PNA)
Source: Philippine News Agency (PNA)
Ayon sa Philippine National Deployment and Vaccination Plan for COVID-19 Vaccines, nakakalap na ang pamahalaan ng ₱82.5 billion. Ilalan ito sa pagbili ng mga vaccine at iba pang mga gastusin sa pagbabakuna.
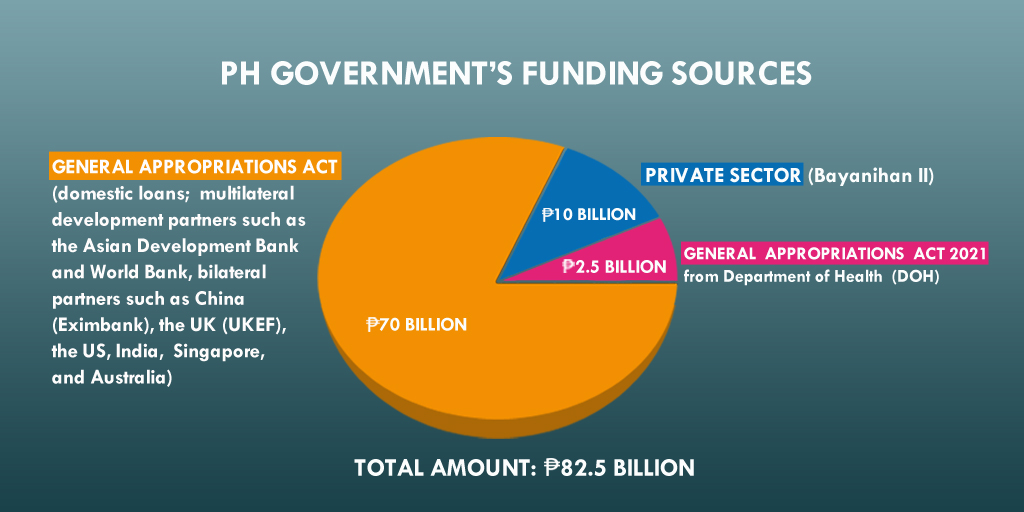 Source: DOH
Source: DOH
Nabanggit ni Department of Finance (DOF) Secretary Carlos Dominguez III na posibleng umabot sa ₱1,300 ang pagbabakuna sa bawat indibiduwal. Dagdag pa niya, mga 57 milyong Pilipino ang makikinabang sa ₱75-bilyong pondong inilaan ng pamahalaan sa pamimili ng mga vaccine. Ang natitirang populasyon ay paggagastusan ng mga LGU (local government unit) at pribadong sektor. Sa ilalim ng Bayanihan to Recover as One Act, pumirma ng kontrata ang lokal na pamahalaan, LGU at mga 300 pribadong kumpanya upang bumili ng 17 milyong dosis mula sa British pharmaceutical company na AstraZeneca. Ayon kay Joey Conception, ang Presidential Adviser for Entrepreneurship, kalahati ng mga dosis na bibilhin ng pribadong sektor ay ibibigay sa gobyerno, habang ang kalahati ay mapupunta sa mga empleyado ng mga kumpanya.
Nationwide Vaccination Drive
 Sources: DOH, WHO, PNA
Sources: DOH, WHO, PNA
 Higit sa 480,000 dosis ng AstraZeneca vaccine ang ibinigay ng COVAX facility sa Pilipinas. (Photo: National Task Force Against COVID-19)
Higit sa 480,000 dosis ng AstraZeneca vaccine ang ibinigay ng COVAX facility sa Pilipinas. (Photo: National Task Force Against COVID-19)
Base sa tinatayang datos ng paglago ng populasyon mula sa Philippine Statistics Authority, bumuo ang pamahalaan ng three-year vaccination plan mula 2021 hanggang 2023. Inaasahan na sa 2022, maaari nang mabakunahan ang mga 16 years old pababa, habang meron nang COVID-19 vaccine para sa mga sanggol sa 2023. Ang mga binakunahan ngayong 2021 ay bibigyan pa ng booster shots sa susunod na mga taon.
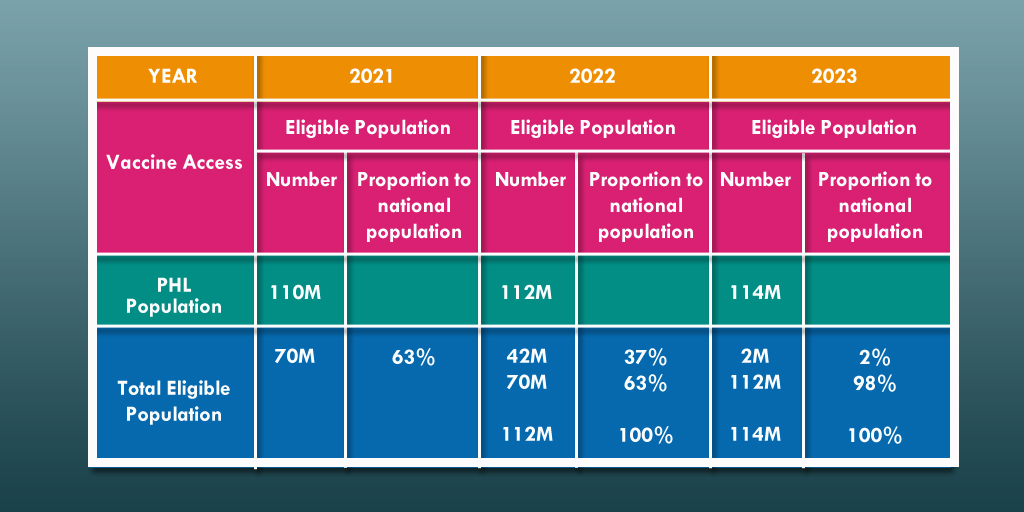 Source: DOH
Source: DOH
Pagkamit ng Herd Immunity
Kahit hindi pa alam ng WHO ang eksaktong porsyento ng isang populasyon na dapat mabakunahan upang makamit ang herd immunity, layunin ng pamahalaan ang mabigyan ng COVID-19 vaccine ang 70 milyong mga Pilipino ngayong 2021. Pero dalawang dosis ang kailangan para makumpleto ang pagpapabakuna— ibig sabihin, 140 milyong dosis ang dapat maiturok ngayong taon.

Base sa mga bilang na ito, dapat bilisan ng pamahalaan ang pagbabakuna para magkaroon ng herd immunity sa bansa—lalo na’t kailangang kailangan na ito ng ating ekonomiya.
Matagal pang haharapin ng bansa ang pandemya, at hindi pa natin alam kung kailan ito matatapos. Ngunit isang bagay ang maliwang: hangga’t hindi pa nababakunahan ang 70 milyong mga Pilipino, kailangan ng ibayong pag-iingat ngayong tumataas muli ang mga kaso ng COVID-19 sa bansa.
Tumatakbo ang oras, pero habang wala pang bakuna ang karamihan ng mga Pilipino, dapat sundin ang mga hakbang upang masiguro ang pansariling kalusugan at kaligtasan. Sa ganitong paraan pa lang natin maiiwasan ang sakit na patuloy na dumadagdag sa 2 milyong bilang na namamatay sa buong mundo.
Never before have we been more dependent on the internet than this pandemic. The virtual space has become a hub for our daily activities—learning, shopping, working, and catching up with friends and family. To foster business continuity, companies have been conducting video conferences instead of face-to-face encounters. Panahon TV is no exception, holding its weekly general assembly online since March.
But if you’ve ever participated in a video conference, you notice how starkly different it is from a real meeting. Participants don’t share the same physical space, which means you see them with different backgrounds, lighting, and video quality. Internet speeds also vary, causing glitches and sudden disconnections. At times, this causes delay and the poor relay of information.
According to this article, experts warn that “distortions and delays inherent in video communication can end up making you feel isolated, anxious and disconnected.” In fact, a 2006 study on remote interpreters at the United Nations and European Union Institutions revealed that after translating discussions via video, they experienced signs of alienation and fatigue because they lacked the “visual perception of the meeting room.”
Because of the challenge of encouraging employee participation in the virtual realm, these simple steps were taken by Panahon TV to make their weekly meetings more enjoyable and engaging.
QOOTD (Quarantine Outfit of the Day) Challenge
Because participants are in the comfort of their own home, and screens only show their upper bodies, they often don’t feel the need to dress up as formally as they would in an office setting. But Visual Consultant Jazel Villamarin would always make an effort to dress up for meetings from head to toe. “Since day one, I would be in full get-up— complete with makeup, accessories, nail polish and shoes. Several virtual meetings later, I was able to persuade everyone to make an effort, hence the QOOTD theme was born.”
At the end of each assembly, Villamarin announces the QOOTD theme for next week’s meeting.
“The themed meetings are like a visual journal that reflects the passage of time. We had themes like ‘Use Your Favorite Bag with Pandemic Necessities” and “Interview Outfit” because we’ve been doing a lot of virtual interviews. For Christmas, our supervising producer gifted us with “I Survived 2020” shirts so we incorporated that into a sporty attire because we all want to be fit and healthy this year. We also had fun themes to lighten up the mood like “Crazy Hats”, “Make Your House Dress More Fashionable”, “Animal Prints”, “Wear Something with Sentimental Value” and so on.”
 The tough gets going: the studio team wearing “I Survived 2020” shirts
The tough gets going: the studio team wearing “I Survived 2020” shirts
Director Julius Melo shares that the themes make online meetings lively and engaging, encouraging employees to look and feel good. “It promotes creativity, and stimulates us mentally, emotionally, and physically. It gives us the chance to open our wardrobe again and put on our favorite clothes and accessories.” Technical Operator Robi Robles enjoys the challenge of putting together ensembles that fit the themes. “If it weren’t for the QOOTD, our general assembly would be boring. Every week, I look forward to seeing my workmates in their unique outfits.”
 Julius, often seen in Nike shirts in the office, elicited gales of shocked laughter when he showed up in an online meeting wearing his wife’s dress during the “Wear Skirt or Formal Pants” theme.
Julius, often seen in Nike shirts in the office, elicited gales of shocked laughter when he showed up in an online meeting wearing his wife’s dress during the “Wear Skirt or Formal Pants” theme.
But the requirement doesn’t end with the outfits; during meetings, employees take turns to explain their reasons for choosing their attire. This brings out their humorous and personal side, allowing them to unload during these difficult times.
For Villamarin, the most memorable theme so far is “Wear Something with Sentimental Value” because of the personal memories that came with the clothes. “Some wore clothes which belonged to loved ones who’ve passed away. I fell in love with the team more after this, and I think it brought us closer like a family.”
 Bon wearing his father’s shirt
Bon wearing his father’s shirt
Case in point is Video Editor Bon Galang, who often keeps quiet during meetings. But when it was his turn to share, he talked about the shirt he wore, which was his father’s. “My dad passed away when I was in high school, and out of the clothes he left, I kept this shirt because it was the only one that fit me. Wearing it brings back my memories of him.” The same QOOTD theme prompted Weather Reporter Patrick Obsuna to wear his family reunion shirt. “Since I was a kid, I was raised by my parents to always put family first, but this pandemic, we weren’t able to conduct our yearly reunion. It made me sad but I remembered the quote that went ‘2020 isn’t the year to count the things you didn’t have, but to be thankful for things you already have.’ Although we weren’t able to see each other this holiday season, there’s another Christmas to look forward to, wherein, hopefully, we can all be together again.”
 Patrick in his family reunion shirt
Patrick in his family reunion shirt
For Executive Producer Donna Lina, these stories are precious. “Some themes are fun, while some—I don’t think we really intended this—managed to show the deeper side of our colleagues. I see another side of them that helps me understand them better.” Villamarin believes that there’s more to the weekly challenge than meets the eye. “Dressing up is a form of self-care; you try to look good for yourself. Judging from the level of participation among employees, I think the QOOTD has successfully fostered teamwork. These are tough times, and we have different ways of coping with daily anxieties. Through this, we get to lighten things up, have fun and enjoy each other’s company albeit virtually.”
 Robi wearing his red hoodie, a gift from his brother.
Robi wearing his red hoodie, a gift from his brother.

COVID-19 barangay updates
The main reason for virtual meetings cannot be escaped. The Panahon TV team tackles this issue head-on by reporting weekly updates of COVID-19 cases in their respective barangays.
Lina, who initiated this practice, believes this is part of being a responsible citizen. “ One way to manage the cases is having an informed and involved citizenry. As our team reports on daily cases on our show and social media platforms, we also make sure that we ourselves are on top of the situation by knowing the cases in our barangay. If these aren’t updated, we nudge our barangays to give us an update.”
 Jearom in his favorite QOOTD theme, “Interview Outfit”
Jearom in his favorite QOOTD theme, “Interview Outfit”
Graphic Artist Jearom Martinez says that the reports let him know “if we are safe in our areas”, while Robi shares that the practice has made him be more vigilant. Meanwhile, Patrick comments: “Aside from learning how our barangays are faring, it also gives us a real grasp on how each barangay is tackling the pandemic.” The learnings from this exchange have given rise to new content, such a critique of the government’s communication techniques during the pandemic.
Recently, updates on the employees’ barangays vaccination plans have been included in the agenda.
Weekly Photo Contest
Though the weekly photo contest, which aims to improve the employees’ visual storytelling skills, is now on its third year in Panahon TV, the viewing of entries remains to be one of the most-awaited portions of the online meetings.
 “Element of Water” by Marmick Julian
“Element of Water” by Marmick Julian
“Continuous improvement is what we’d like to see here,” Lina says. “The photo contest is both an engagement and educational activity. Through this exercise, we’ve upskilled our members coming from computer science and journalism to be more visual.”
Each week, Villamarin choses a theme for the photo exercise. “Photos taken during the pandemic are more personal and intimate because we are all spending a lot more time at home and with our families.” Instead of being the sole contest judge, Villamarin has begun selecting only the top three entries, and letting the previous week’s winner choose the best photo. “This new process came from an employee’s suggestion, so the team can practice critical thinking.”
 “Dawn” by Patrick Obsuna
“Dawn” by Patrick Obsuna
For the employees, the photo exercise is a welcome challenge. “It pushes me to study composing the photo before taking it,” shares Bon. For Jearom, it doesn’t only improve his skills, but also “reduces my anxiety during the pandemic.” Robi is able to apply his learned skills as a communications graduate, while Patrick has observed his improvement in creative visual expression. “I got better in framing and choosing an angle for my subjects. Aside from looking at the photo entries, I also enjoy hearing the funny explanations my co-workers share about their photos. This lessens my emotional burden from the pandemic. I think the fun and hilarious things we do in our meetings are due to the fact that we’re like family—this is why we’re comfortable in expressing our feelings and keeping our mental health in check.”
 “Shape of You” by Raffy Vicente
“Shape of You” by Raffy Vicente
Villamarin agrees. “It’s nice to hear them give feedback on each photo, and in a way, we get to know each other more. It’s a pleasant surprise to hear their interesting points of view.” She ends, “I believe these QOOTD-themed virtual meetings and photo assignments are a way of taking care of each other. They give proof of life that we survived 2020 together, and that we are here for each other.”
 Employees in “Sporty Attire” theme
Employees in “Sporty Attire” theme
